People sometimes seem to wonder why I speak and write so regularly about the experience of an unexpected patient outcome and medical malpractice litigation. Even though there is too little support for doctors facing a malpractice lawsuit, it strikes some people as peculiar for a practicing physician to get up and tell a personal story of this aspect of medical practice. Perhaps I can explain why I do it by giving you an analogy.
Speak Out and Change the World
When I was a young girl, First Lady Betty Ford spoke out and changed the world. She lived in a time when people simply did not talk about having breast cancer. It felt shameful to them. And because it was not an acceptable topic for conversation, women's lives were needlessly lost.
First Lady Betty Ford, age 3 — a little girl who grew up to change the world
Betty Ford, however, broke the mold. She found a lump in her breast and was diagnosed with cancer. She underwent a total mastectomy in a time before breast reconstruction was the norm. She openly revealed her diagnosis and the nature of her surgery, and was even candid about her worries that her husband Gerald's feelings toward her would change.
No one would have blamed her had she chosen to keep things confidential. However, given that her diagnosis followed so closely upon Watergate and Nixon's resignation, I believe she recognized the nation's need for truthfulness from the White House. Her honesty and her promotion of mammograms completely changed the world for the 1 in 8 women and the lesser number of men diagnosed with breast cancer.
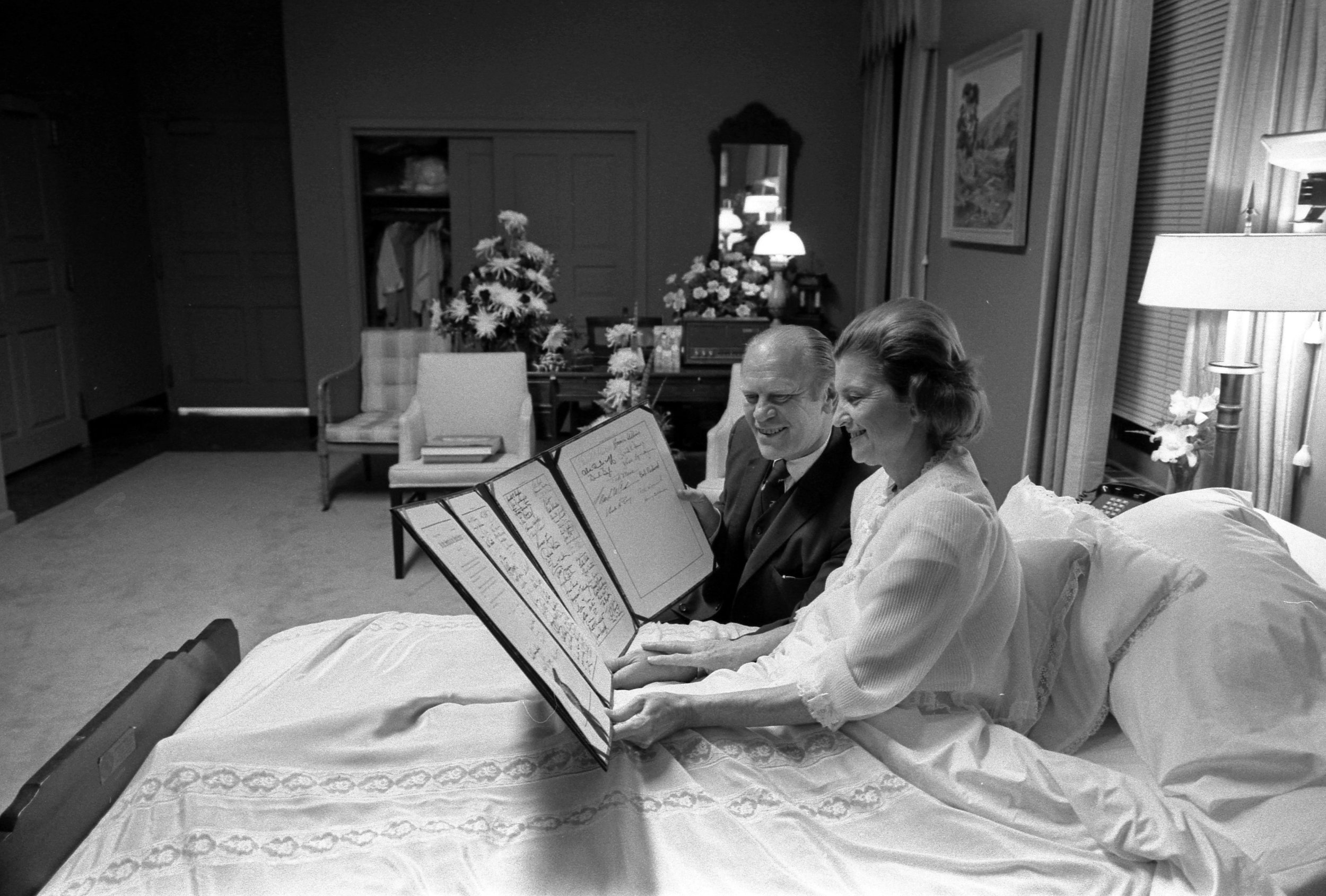
First Lady Betty and President Gerald Ford at Bethesda Naval Hospital after her surgery. October, 1974
Among physicians, as I've written before, far more than 1 in 8 face malpractice litigation. The best study I've found to date suggests that, by the age of 65, 75% of doctors in “low-risk” specialties and 99% in “high-risk” specialties will be named in a lawsuit. I'd say we're all high risk then, wouldn't you?
The fact that the majority of us will be sued doesn't make it any easier for us than a diagnosis of cancer would be. Most physicians who have survived a lawsuit – and I am one of them -- will tell you that recovering after a patient's unexpected outcome and living through malpractice litigation is the hardest thing they have ever done, without exception.
In some specialties, physicians are sued on average once every 5-8 years. This is not hypothetical. I have worked alongside excellent physicians, out there taking risks every day to address our childbirths or emergencies or perform complex surgical procedures, whose professional experience is precisely that.
Effects of Lawsuits on Physicians
In the world of emergency medicine, we are so aware of the heroics performed by the trauma teams who responded to the Boston Marathon bombing, the Pulse Nightclub tragedy, the Las Vegas shooting. We see that those events take a toll on them, we're dazzled by their tenacity and skill in a crisis, and we are proud that they are our own.
On some other day, however, I assure you, those selfsame trauma surgeons, emergency physicians, and trainees are being sued. And I believe that takes an equally profound or greater toll on them, their health, and their ability to practice their profession.
We physicians and other healers are not so different from folks in Betty Ford's day. Sure, we speak freely about cancer now, but we have a deeply entrenched taboo against discussing our experiences with medical malpractice litigation even within our community. It makes us feel ashamed, and we may feel anxious that our colleagues will not trust us to take good care of their patients.
Consequently, I'll bet that many physicians among you cannot tell me which of your colleagues has had this deeply personal experience. It is my view that this taboo harms us, and in harming us, it harms the patients we serve. I speak and write about this aspect of our lives in the hopes of doing a Betty Ford.
Adverse Effects on Doctors of Adverse Patient Outcomes
Just like cancer, our silence around such a tough experience has the potential to take physicians and other healers' personal and professional lives from them, their families, and their patients, figuratively and literally. As I've often mentioned, the experience of adverse or near-adverse outcomes and litigation is widely known to result in PTSD in practice. It drives some physicians to retire early – go into some other profession, say. Or, they may leave the operating room which they had loved and pursue a non-clinical role, often at the mid-point of their career when their clinical know-how is right at its peak. Given that we face physician shortages which the AAMC projects to reach as many as 120,000 by the year 2030, the loss of their years of clinical experience should worry us all.
We have all known physicians affected by painful patient outcomes and malpractice litigation who gave up OB to practice gynecology alone. I do not criticize any of these choices; my colleagues make them out of their suffering, and I considered them myself. However, I do think it is worth recognizing that no fewer babies are born and no fewer patients require surgery than the day before a physician makes the choice to leave a clinical skillset behind.
These experiences affect healers' physical health, and no small number experience depression and even suicide. In fact, it was in the midst of my own trial a few years ago when I stumbled quite by chance upon a TED talk on the topic of physician suicide that I started out on the path that has brought me here.
Malpractice Litigation and Physician Identity
You know, there are also other parallels to Betty Ford's experience. Her diagnosis of cancer had to be very hard. Losing a breast touches deeply upon many women's sense of their essential identity, while cancer generally has the potential to interrupt a person's confidence that they are safe in the world. Likewise, an unforeseen adverse outcome and ensuing medical malpractice lawsuit is crushing for many doctors. Not unlike a cancer diagnosis, it can feel like an emergency which persists for years.
To quote the US Navy's old advertisement, this work is “not just a job,” for many of us, “it's an adventure.” We make a unique array of sacrifices to learn the art and science of medicine, and the experiences we encounter along the way often weave our identity as a healer into our very fiber. Most of us embrace this work not as “what we do,” but rather “who we are,” and we don't really want it any other way. For a time, my own patient's unforeseen death and the medical malpractice lawsuit which followed challenged essential features of my identity as a person who protects the young, someone with significant clinical insight accumulated over time, and it ruptured my confidence that I was safe in a world I love.
As I engage in public speaking and explore creative ways to provide support for physicians facing a bad patient outcome or malpractice lawsuit, I am continually touched by the passionate responses of physicians of every age and professional stage. Even malpractice defense lawyers, healthcare risk managers, and other healthcare professionals seem relieved to explore these tough issues.
Just like Betty Ford and mammograms, our conversations can result in our healing and change our world. I hope you'll join the conversation.
A variation on this post appeared in a talk I gave last April as the Miles and Elena Zaremski lecturer hosted by the Health Law Center at Case Western Reserve University’s School of Law, one of the top five Health Law programs in the nation. An edited version of that presentation will be published in Spring, 2019, in HealthMatrix, the CWRU journal of Health Law. You can view that presentation here (starts at about 15:00).